Giving Elders a Voice in Their Own Care: Person-Centered Care and Choice
Person-Centered Care puts considerable value on an individual’s right to make decisions concerning every aspect of her or his life. Often long-term care providers want to honor resident choice, but are afraid to do so because of fear of injury or risk of liability. The key is to find the balance between providing good care and keeping elders safe, on the one hand, and allowing choice which may involve risk but enhances quality of life, on the other.
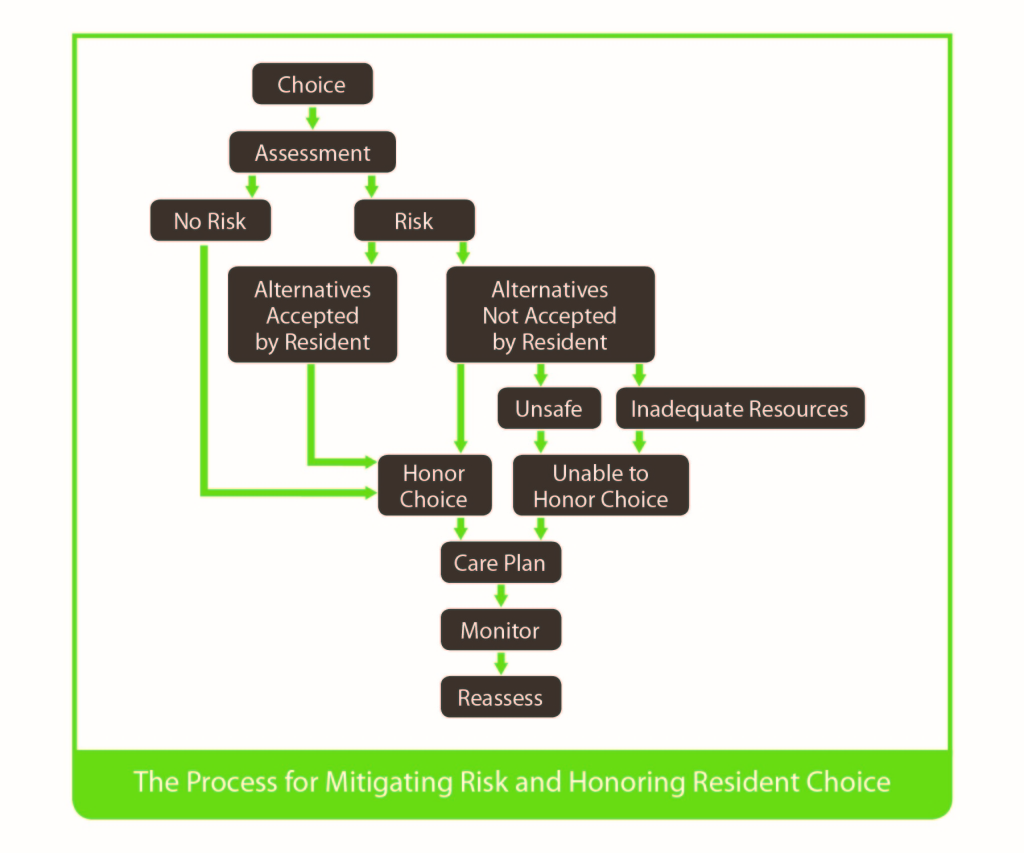
So how does the care community accommodate resident preferences when the choice is seen as having some potential risk for a negative outcome?
The Rothschild Person-Centered Care Planning Task Force, sponsored by the Hulda B. and Maurice L. Rothschild Foundation, worked for over a year to create A Proposed Process for Care Planning for Resident Choice. I was involved as a member of the steering committee that created and guided the work of the task force. I would like to share some information about this process, which is specifically aimed at care planning when the choice carries sufficient risk and the community is considering not honoring the resident’s wishes. Following the process summarized below will help the community work with the elder to understand and respect choices to the greatest extent possible.
Step 1: Identify the Choice
Talk with the elder and gather as much information about the nature of the choice that the person wishes to make. Repeat back to the person your understanding of what she or he desires to choose or refuse, to confirm both parties understand each other.
Step 2: Discuss the Options
Discuss potential positive and negative outcomes of respecting his or her choices, as well as the potential outcomes of preventing the person from acting on the choices. The care team should offer ways in which they can accommodate the choice and also mitigate potential negative consequences.
Step 3: Determine how to Honor the Choice
While some requests are potentially too harmful to other people to honor, many other requests can and should be honored by creating a plan to mitigate known potential negative consequences or offering a similar activity which has fewer potential adverse consequences. The team should compare the elder’s choice to the person’s condition to determine the nature of potential risks. If the requested action poses significant danger to others, the team should clearly explain why they cannot honor that particular choice.
Step 4: Care Plan the Choice
If a mutual decision is reached as to how the team will accommodate a choice to maximize the elder’s well-being, the team will work out with the person the specific steps the staff will take to support that choice. The elder participates in the care planning process and is made aware of the steps of the plan.
Step 5: Monitor and Make Revisions
Monitor the progress of the plan and its effects on the elder’s well-being and ongoing desire to continue with the choice. The team will work with the person to revise the plan as needed and desired by the resident. Care plans and staff should be flexible, as people have the right to change their minds.
Step 6: Quality Assurance and Performance Improvement
The Quality Improvement team should review trends related to resident choice and safety, particularly when elders are routinely denied requests, or when the team identifies patterns of community care practices that might be improved by performance improvement action plans.
Summary
For so long, the focus in long-term care has been on doing what is “in the best interest of the person” as defined by the healthcare professional staff, rather than as defined by the person. In contrast, this care planning process has been developed to help give the person a voice in directing his or her own care. Rather than viewing a person as non-compliant if he or she does not agree with your recommendations, try viewing the elder as a member of the care team participating in the discussion about options, potential risks and outcomes.
The full Process for Care Planning for Resident Choice, which includes blank forms and case studies can be found at https://brushdevelopment.com/wp-content/uploads/2015/09/Care_Planning_for_Resident_Choice_070915.pdf






